I hope you enjoyed reading through the blog and had a chance to think about the broad pictures of some of the social determinants that impact obesity and the associated comorbid conditions. The reason I chose to do this assignment in blog format was to explore a different way of expressing and synthesizing information that is found on the health topics that we are researching. Social media allows health care professionals to access new forms of intervention and health promotion strategies that have not been allowed conventionally. It also gave me an opportunity to compare the things that I was reading about in academic journals with how these things play out in my own environment. Finally, use of this format gives me the freedom to synthesize different sources of information, from news articles, Youtube, other blogs etc.(things the general public uses and is familiar with) into this assignment.
Please feel free to give feedback and comments on what you think about the issues and arguments I have included here.
Monday, April 19, 2010
Why This Matters
Traditional approaches of combating obesity have often consisted of health care professionals encouraging individuals to eat less and exercise. This has led to a multi-billion industry revolving around dieting and intense exercise routines that are difficult for people to incorporate into their daily lives. Meanwhile, despite these efforts, the rates of obesity have continued to increase.
The Heart and Stroke Foundation of Canada released a position statement calling for different levels of governments, policy makers, and Canadians to get involved in creating healthier environments. For instance, strategies to change the built environment to promote walking impact our health have been advocated for. The article describes that the risk of obesity "can decline by 4.8% for each additional kilometre walked per day".
The Heart and Stroke Foundation of Canada released a position statement calling for different levels of governments, policy makers, and Canadians to get involved in creating healthier environments. For instance, strategies to change the built environment to promote walking impact our health have been advocated for. The article describes that the risk of obesity "can decline by 4.8% for each additional kilometre walked per day".
New York City has taken some of the research on the built environment and the importance of involving non-traditional stakeholders to heart, and has developed strategies to promote a healthier city through. The New York Fit City project couples the health department with non profits, community groups, and academic institutions. Over the short span the project has been running, they have documented significant improvements in dietary patterns and physical activity. The initiatives range from opening community gardens to changing building designs and having stair prompts beside elevators. Such imaginative strategies are inspiring and serve as good models for seeing the research being translated into action to improve health for people.
Putting it all together
From all the different posts that I have included in this blog, it is clear that obesity and the associated comorbid conditions is a complicated problem with a very complex etiology. The following chart was presented to our class in a lecture from Dr. Arya Sharma, that captures the complexity of the situation quite well:
I could go on describing each one of these factors and how they impact obesity. The big picture to consider is the same one that we hear numerous times regarding many different conditions: "Genetics loads the gun, and environment pulls the trigger." The tremendous rise in obesity and associated comorbidities begs health care providers, policymakers, and the general society to consider interventions that address the issue in a broad manner, rather than blaming the individual and reducing the debate to simply being a matter of over eating and energy balance.
Research indicates that broad issues such as socioeconomic status, the built environment, and changes in dietary patterns have all contributed to the rising prevalence of obesity. In addition, these factors do not impact obesity in isolation. They overlap and influence each other, and greater understanding of these relationships is required to enhance our ability to create meaningful interventions. Considering obesity from a multi-factorial model also allows us to use a bigger toolkit aiding with prevention and management strategies. For instance, considering addiction to food as a cause of obesity among some people, and use of strategies used among mental health and addiction issues may be worthwhile to consider.
It is also important to remember that health care workers and policymakers will need to integrate information and strategies from different professions to make future interventions more successful. We need to be able to draw from diverse backgrounds ranging from architects and civil engineers involved in building design and urban planning to nutritionists and physicians to tackle the deficits in health that are created by our environment.
I could go on describing each one of these factors and how they impact obesity. The big picture to consider is the same one that we hear numerous times regarding many different conditions: "Genetics loads the gun, and environment pulls the trigger." The tremendous rise in obesity and associated comorbidities begs health care providers, policymakers, and the general society to consider interventions that address the issue in a broad manner, rather than blaming the individual and reducing the debate to simply being a matter of over eating and energy balance.
Research indicates that broad issues such as socioeconomic status, the built environment, and changes in dietary patterns have all contributed to the rising prevalence of obesity. In addition, these factors do not impact obesity in isolation. They overlap and influence each other, and greater understanding of these relationships is required to enhance our ability to create meaningful interventions. Considering obesity from a multi-factorial model also allows us to use a bigger toolkit aiding with prevention and management strategies. For instance, considering addiction to food as a cause of obesity among some people, and use of strategies used among mental health and addiction issues may be worthwhile to consider.
It is also important to remember that health care workers and policymakers will need to integrate information and strategies from different professions to make future interventions more successful. We need to be able to draw from diverse backgrounds ranging from architects and civil engineers involved in building design and urban planning to nutritionists and physicians to tackle the deficits in health that are created by our environment.
And the list goes on...
It's Addictive:
 A few weeks ago, the Edmonton Journal had a news story about high fat foods leading to addiction. In it, the Journal described a study that explored the re-hardwiring of rat brains that led to their dependence on high fat foods. Dr. Valerie Taylor and her colleagues have explored addiction to certain components of food, where people develop tolerance to food, and require increased "dosage" to maintain satiety. According to Taylor, many of the characteristics of intake and withdrawal are consistent in certain individuals with other addictive substances. If you are looking for a more scientific explanation, it seems that high calorie foods may lead to down-regulation of dopamine D2 receptors linking them to addictive behaviours.
A few weeks ago, the Edmonton Journal had a news story about high fat foods leading to addiction. In it, the Journal described a study that explored the re-hardwiring of rat brains that led to their dependence on high fat foods. Dr. Valerie Taylor and her colleagues have explored addiction to certain components of food, where people develop tolerance to food, and require increased "dosage" to maintain satiety. According to Taylor, many of the characteristics of intake and withdrawal are consistent in certain individuals with other addictive substances. If you are looking for a more scientific explanation, it seems that high calorie foods may lead to down-regulation of dopamine D2 receptors linking them to addictive behaviours.Broadening the search for the etiology of the obesity epidemic has helped Taylor and others develop new approaches and strategies. Although this is not true for the general population, for numerous individuals struggling with obesity, use of behavioral therapy, along with evidence and techniques that have been learned in dealing with other addictions can be applied in the treatment model for obesity.
H/t to Rohan Parab for pointing this out to me. Here is a movie coming up "Lbs" that follows two friends, one dealing with food addiction and another with crack.
Is it the gym teachers fault?
 Did you have a bad experience in gym while growing up? In his research on early childhood experiences in physical education, Dr. Billy Strean found that up to 45% of kids were called names and teased during play time as kids. Many kids were excluded from physical activity and unvalued by teachers and coaches. These early experiences can have lifelong implications in the person's physical activity profile as an adult. Strean calls for an increased emphasis on developing skills, and making physical activity enjoyable and fun for children, rather than focusing on performance. Strean's research indicates that addressing and using educators to increase participation and sustainability of physical activity can have positive influences on reducing childhood and adult obesity in the future!
Did you have a bad experience in gym while growing up? In his research on early childhood experiences in physical education, Dr. Billy Strean found that up to 45% of kids were called names and teased during play time as kids. Many kids were excluded from physical activity and unvalued by teachers and coaches. These early experiences can have lifelong implications in the person's physical activity profile as an adult. Strean calls for an increased emphasis on developing skills, and making physical activity enjoyable and fun for children, rather than focusing on performance. Strean's research indicates that addressing and using educators to increase participation and sustainability of physical activity can have positive influences on reducing childhood and adult obesity in the future!Head to Head: Chips vs. Carrots?
A review on the role of energy density and food costs by Adam Drewnowski and SE Specter, reveals that there is an established relationship between the low cost of calorie-rich foods. People are getting higher percentage of their calories from energy dense foods (high in fat and sugar). Meanwhile the volume of food we eat has remained about consistent. Moreover, energy dense food are more palatable and influence preference of dietary tastes.
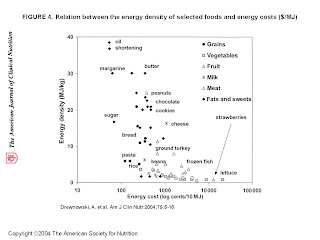
Over the past few decades, the cost of energy-dense foods has become very low. For instance, the energy cost of potato chips was about 20cents/MJ(1200kcal/$) while fresh carrots were about 95 cents/MJ(250kcal/$). Energy dense foods have been increasing in the mainstream diet readily over the past few decasdes, and cost for these foods has increased much slower than it has for healthier options of fruits and vegetables. Diets which include a lot of these energy dense, unhealthy options have been linked with higher risks of developing type 2 diabetes and obesity.
The review also revealed that income affects the quality of foods people eat, with higher SES groups having better quality diets. Food costs were found to be an issue for low income families as they spend a higher percentage of their disposable income on food.
This review demonstrates that there are broad factors at play when explaining the rise of the obesity epidemic. The study reveals that cost of food, access to income, how our palate and biopsychological dietary patterns develop based on the energy density of foods, confluence together to influence the rise in obesity!

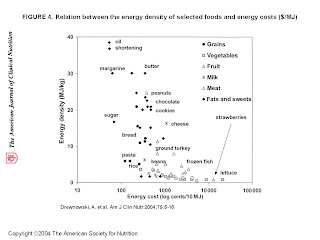
Over the past few decades, the cost of energy-dense foods has become very low. For instance, the energy cost of potato chips was about 20cents/MJ(1200kcal/$) while fresh carrots were about 95 cents/MJ(250kcal/$). Energy dense foods have been increasing in the mainstream diet readily over the past few decasdes, and cost for these foods has increased much slower than it has for healthier options of fruits and vegetables. Diets which include a lot of these energy dense, unhealthy options have been linked with higher risks of developing type 2 diabetes and obesity.
The review also revealed that income affects the quality of foods people eat, with higher SES groups having better quality diets. Food costs were found to be an issue for low income families as they spend a higher percentage of their disposable income on food.
This review demonstrates that there are broad factors at play when explaining the rise of the obesity epidemic. The study reveals that cost of food, access to income, how our palate and biopsychological dietary patterns develop based on the energy density of foods, confluence together to influence the rise in obesity!

Does Sobeys Urban Fresh Change the Way You Eat?
 The last post about how supermarkets impact our dietary trends got me thinking of how our own community measures up. Although I don't want to promote a specific brand of grocery stores, I think the way that Sobeys has integrated Urban Fresh Markets in settings which are filled with convenience stores, fast food outlets, and restaurants provides a healthier and convenient option for people to access healthier alternatives. There are two of these stores, one on Jasper Ave, and the other near University of Alberta. Although I am unsure of how cost effective is to shop at these stores, I think it's a good step in integrating supermarkets and healthy food options into day to day food outlets.
The last post about how supermarkets impact our dietary trends got me thinking of how our own community measures up. Although I don't want to promote a specific brand of grocery stores, I think the way that Sobeys has integrated Urban Fresh Markets in settings which are filled with convenience stores, fast food outlets, and restaurants provides a healthier and convenient option for people to access healthier alternatives. There are two of these stores, one on Jasper Ave, and the other near University of Alberta. Although I am unsure of how cost effective is to shop at these stores, I think it's a good step in integrating supermarkets and healthy food options into day to day food outlets.I am curious to see if people living or working near the U of A have noticed any changes in their dietary trends since the opening of the place a couple years ago?
Creating capacity for healthy foods in our community is an important step in how people choose their diets. Adding readily accessible foods, especially in disadvantaged communities has been succesful in many different communities such as in California, and perhaps should be tried as a strategy to reduce the risk of obesity in low SES communities.
Sunday, April 18, 2010
How We Eat
As mentioned before fast food outlet density is related to increased risk of obesity. On the flipside, access to supermarkets offering a variety of high-quality products, especially at lower costs seems to be associated with a risk reduction in obesity. The review conducted by Dr. Nicole Larson et. al on neighbourhood environment and access to healthy foods found interesting results relating to this area.
- Each additional supermarket was related to a 32% increase in predominantly African-American communities and 11% increase in predominantly Caucasian in meeting fruits and vegetable guidelines.
- A study in the review also found that fruit and vegetable intake in kids was related to the distance between home and nearest convenience store.
- Residents of rural, low income, and minority communities were at higher risk of obesity due to poor access to supermarkets, healthy food stores, and other grocery stores.
Eating Out
Eating Out
What's interesting about the review was that it examined the patterns of our dietary intake as well, and found that eating out at restaurants accounts for about half the US food expenditures(~$558 billion). Eating out, particularly at fast food restaurants, is associated with greater prevalence of obesity. In addition, restaurant meals tend to higher in calories and lower in nutritional quality, contributing to an unhealthy diet. I mentioned some of the relationships earlier, but Larson et. al have described studies that show a much more subtle dynamic at play with regards to placement of fast food restaurants and low income communities. Lower SES communities tended to have higher density of fast food outlets. In addition, richer communities had higher proportion of healthy food choices offered on their menus compared to lower SES communities.
These differences add up and contribute to how the obesity epidemic manifests itself in different communities!
A word about co-morbidities
The links between obesity and other comorbid conditions has been well established in the literature, and the list of associated problems related to obesity is immense. For instance, there is a strong link between obesity and Type 2 diabetes, where obesity contributes to insulin resistance and an increased risk of developing Type 2 diabetes. The rise of type 2 diabetes in children and global increases in the disease prevalence demonstrates the health, social, and economic strains that these cluster of conditions will create. For instance in the United States, diabetes costs have arisen to over $100 billion. Many of the same trends and risk categories seem to apply to diabetes as they do to obesity.
The following is from a slide in an Endocrine lecture our class received from Dr. Ellen Toth which describes a stark difference in obesity rates based on SES in a small geographic area. The East Harlem area has the highest rates of diabetes in the city while Upper East side manhattan has the lowest rates, all within a few blocks of each other...


The following is from a slide in an Endocrine lecture our class received from Dr. Ellen Toth which describes a stark difference in obesity rates based on SES in a small geographic area. The East Harlem area has the highest rates of diabetes in the city while Upper East side manhattan has the lowest rates, all within a few blocks of each other...


Disclaimer: A Word of Caution - Association vs Causation
I just wanted to back up for a moment and talk about association vs causation. I myself had a lot of trouble with this when I first learnt about it, and I think it's worthwhile to mention it here. Most of the studies that I have cited here do not use randomized controlled trials because of it is unfeasible and impractical to do such studies on the environmental scale that I am considering risk factors for obesity and comorbid conditions.
 Association or correlation basically means that there is a trend that seems to go along with another trend. So for example, one of the things that obesity seems to be related to is a lower socioeconomic status in a community. However this is an association and not a causation. The studies that have found this out are observational studies, and you cannot find out about causation from these studies.
Association or correlation basically means that there is a trend that seems to go along with another trend. So for example, one of the things that obesity seems to be related to is a lower socioeconomic status in a community. However this is an association and not a causation. The studies that have found this out are observational studies, and you cannot find out about causation from these studies.
 Association or correlation basically means that there is a trend that seems to go along with another trend. So for example, one of the things that obesity seems to be related to is a lower socioeconomic status in a community. However this is an association and not a causation. The studies that have found this out are observational studies, and you cannot find out about causation from these studies.
Association or correlation basically means that there is a trend that seems to go along with another trend. So for example, one of the things that obesity seems to be related to is a lower socioeconomic status in a community. However this is an association and not a causation. The studies that have found this out are observational studies, and you cannot find out about causation from these studies.Causation requires researchers to conduct experimental studies that control for variables, and have control groups to compare a certain experimental or intervention group. So for example, one of the studies talked about having specialty coffee shops having a protective associative effect on risk of obesity. This is only a correlation and does not mean specialty coffee shops will prevent obesity. The study needs to be accounted for by other explanations such as the fact that specialty coffee shops are often more densely placed in communities with higher SES demographics.
Saturday, April 17, 2010
More on Fast Food
Edmonton seems to be a great hub for obesity research, and demonstrating the affect of broader factors contributing to obesity. Sean Cash and others from U of A consider the relationshiops between prevalence of obesity and access to fast food restaurants in a given area. The positive correlation between fast food density and obesity has been described in different communities in the states. In addition, lower SES communities and schools and universities tend to have a higher density of these outlets!
Cash and his colleagues compared the location of the top 10 fast food restaurants(Tim Hortons, Subway, McDonald’s, KFC, A & W, Dairy Queen, Harvey’s, Wendy’s, Burger King, and Domino’s Pizza) across Canadian metropolitan cities to explore the difference in adult obesity rates across Canadian cities, which ranged from 11.7%(Vancounver) to 36.4%(St.John's).
The data collected supported that fast food restaurants were positively correlated to obesity rates. Meanwhile, increased specialty coffee shops were associated negatively with obesity. This is accounted by the fact that specialty coffee shops often attract more educated, higher SES status people to a neighbourhood, who have a protective elements from obesity.

Cash and his colleagues compared the location of the top 10 fast food restaurants(Tim Hortons, Subway, McDonald’s, KFC, A & W, Dairy Queen, Harvey’s, Wendy’s, Burger King, and Domino’s Pizza) across Canadian metropolitan cities to explore the difference in adult obesity rates across Canadian cities, which ranged from 11.7%(Vancounver) to 36.4%(St.John's).
The data collected supported that fast food restaurants were positively correlated to obesity rates. Meanwhile, increased specialty coffee shops were associated negatively with obesity. This is accounted by the fact that specialty coffee shops often attract more educated, higher SES status people to a neighbourhood, who have a protective elements from obesity.

Something Closer to Home
Although this might be beating the point that the built environment and SES impact risk factors for obesity to death, but the evidence was also replicated in Edmonton by Dr. Tanya Berry and others from University of Alberta.
Over a six year longitudinal study, the authors found that a younger age and living in a lower SES neighbourhood significantly predicted increased BMI. There was lower neighbourhood satisfaction and higher BMIs in communities with lower incomes. The study also found that the biggest gains in obesity were among young adults, between the ages 18-34.
However, longitudinally, the authors found little change between BMI and walkability of neighbourhoods. This was interestingly attributed to healthier people self-selecting more walkable neighbourhoods, which means that longitudinally there would be low impact on BMI changes. There were components to lower socioeconomic neighbourhoods that contributed to increased obesity.
Over a six year longitudinal study, the authors found that a younger age and living in a lower SES neighbourhood significantly predicted increased BMI. There was lower neighbourhood satisfaction and higher BMIs in communities with lower incomes. The study also found that the biggest gains in obesity were among young adults, between the ages 18-34.
However, longitudinally, the authors found little change between BMI and walkability of neighbourhoods. This was interestingly attributed to healthier people self-selecting more walkable neighbourhoods, which means that longitudinally there would be low impact on BMI changes. There were components to lower socioeconomic neighbourhoods that contributed to increased obesity.
Saturday, April 10, 2010
How Neighbourhoods Fit In
As mentioned before, it is evident that the type of built environment you live in affects the risk of obesity. Studies conducted on different neighbourhoods further support this claim. A study by CE Joshu et. al examined the relationship between personal barriers and neighbourhood barriers for risk factors of obesity. Probably a no-brainer to most, both increased personal and neighbourhood barriers correlated with increased odds of obesity.
The sub-analysis conducted describes interesting results for how built environments impact obesity. The study showed that neighbourhood barriers and personal barriers differed based on the level of urbanization in a community. The personal barriers to living a healthy in all communities that the study was conducted in, were similar in frequency. However here are some differences in how personal and neighbourhood characteristics varied in their impact on obesity across different levels of urbanization, and some explanations:
- Metropolitan: High traffic
The authors also considered macro-level impact of urbanization and how that related to personal and neighbourhood barriers on impact of risk for obesity. There was a higher community sprawl related to higher incidence of obesity, and the risk of this association increased with increased number of personal barriers. Joshu et. al attribute this to the interplay that takes place in development of personal barriers to a healthy lifestyle and the environment one lives in. Environments conducive to a healthy lifestyle (more likely to be compact and low sprawl communities) help to offset personal barriers and other risks of obesity.


The sub-analysis conducted describes interesting results for how built environments impact obesity. The study showed that neighbourhood barriers and personal barriers differed based on the level of urbanization in a community. The personal barriers to living a healthy in all communities that the study was conducted in, were similar in frequency. However here are some differences in how personal and neighbourhood characteristics varied in their impact on obesity across different levels of urbanization, and some explanations:
- Rural Resident: Poor health, dislike of exercise, fear of injury. Lack of sidewalks, concerns about traffic safety, absence of streetlights,reduced access to assistance in event of an injury
Possible explanation: Higher proportion of older adults live in rural areas. Some personal barriers can be explained by neighbourhood ones
- Micropolitan: No time for exercise and being self conciousPossible explanation: Higher proportion of older adults live in rural areas. Some personal barriers can be explained by neighbourhood ones
- Metropolitan: High traffic
The authors also considered macro-level impact of urbanization and how that related to personal and neighbourhood barriers on impact of risk for obesity. There was a higher community sprawl related to higher incidence of obesity, and the risk of this association increased with increased number of personal barriers. Joshu et. al attribute this to the interplay that takes place in development of personal barriers to a healthy lifestyle and the environment one lives in. Environments conducive to a healthy lifestyle (more likely to be compact and low sprawl communities) help to offset personal barriers and other risks of obesity.


Friday, April 9, 2010
A Taste of Campus
I went around HUB, 112th street, and SUB to find out what's available for food on campus. Here's a collage of what I found out.
Maybe this is a giveaway considering University of Alberta is a Coke sponsored university, but I was suprised at how much fast food we have in such a small area of the campus where most students buy their lunch or go for snacks.
In HUB Mall Strip, I counted 20 places where food was the primary commodity, and most of the places had fast or junk food being sold. This means that one out of every three shops sold junk food the entire mall.

Here is a collage of the photos from around campus about the "variety" of foods that are available for students to purchase.
Maybe this is a giveaway considering University of Alberta is a Coke sponsored university, but I was suprised at how much fast food we have in such a small area of the campus where most students buy their lunch or go for snacks.
In HUB Mall Strip, I counted 20 places where food was the primary commodity, and most of the places had fast or junk food being sold. This means that one out of every three shops sold junk food the entire mall.

Here is a collage of the photos from around campus about the "variety" of foods that are available for students to purchase.
Wednesday, April 7, 2010
Incorporating Physical Activity into Daily Life
Here is an example of how to incorporate physical activity into the daily routine. In Stockholm, they were able to increase stair usage by 66% through a simple intervention. Check it out.
Enjoy:
 Can you imagine if stairs were more central in LRT stations rather than just the escalators. I have included some pictures from the University LRT Station for comparison! When I went around with my camera to the platform, it was evident that the escalator was the central focus, and the usage of stairs was almost discouraged:
Can you imagine if stairs were more central in LRT stations rather than just the escalators. I have included some pictures from the University LRT Station for comparison! When I went around with my camera to the platform, it was evident that the escalator was the central focus, and the usage of stairs was almost discouraged:
If you compare the "walkability" of these two options, the escalators are more inviting and safer for one to go upstairs from the platform. The stairs are sort of hidden away at the end of the platform, and they seem a bit unsafe compared to the escalators due to the fact they are secluded. Also, the staircase door has a sign saying "Long Stairwell" - reinforcing the discouragement of their use. This reflects the proportion of people who are taking the escalator rather than the stairs!
Enjoy:
 Can you imagine if stairs were more central in LRT stations rather than just the escalators. I have included some pictures from the University LRT Station for comparison! When I went around with my camera to the platform, it was evident that the escalator was the central focus, and the usage of stairs was almost discouraged:
Can you imagine if stairs were more central in LRT stations rather than just the escalators. I have included some pictures from the University LRT Station for comparison! When I went around with my camera to the platform, it was evident that the escalator was the central focus, and the usage of stairs was almost discouraged:If you compare the "walkability" of these two options, the escalators are more inviting and safer for one to go upstairs from the platform. The stairs are sort of hidden away at the end of the platform, and they seem a bit unsafe compared to the escalators due to the fact they are secluded. Also, the staircase door has a sign saying "Long Stairwell" - reinforcing the discouragement of their use. This reflects the proportion of people who are taking the escalator rather than the stairs!
Tuesday, April 6, 2010
KATZ vs MSB
One of the things that inspired me to write about the built environment was seeing the difference urban design and architecture can have on the amount of physical activity you can incorporate into your life. You might be about wondering what building design has to do with physical activity.
Traditional physical activity programming has pushed for people to start exercising and going to the gyms more frequently. To be a more viable and succesful strategy for healthy living, physical activity needs to be integrated into our day to day lifestyle. This includes having more side walks, more readily visible signs to suggest taking stairs, and having open and accessbile staircases in buildings.
An example of this can be seen in the couple buidlings that our classes are held in, the Medical Sciences Building (MSB) and the Katz Building (KATZ):
Although this is not a quintessential solution to the obesity epidemic, reconsidering how buildings and our urban environments are built has huge implications in our health. There are some municipalities that have embraced such action and have benefited tremendously from it.
Traditional physical activity programming has pushed for people to start exercising and going to the gyms more frequently. To be a more viable and succesful strategy for healthy living, physical activity needs to be integrated into our day to day lifestyle. This includes having more side walks, more readily visible signs to suggest taking stairs, and having open and accessbile staircases in buildings.
An example of this can be seen in the couple buidlings that our classes are held in, the Medical Sciences Building (MSB) and the Katz Building (KATZ):
MSB:
KATZ:
Although this is not a quintessential solution to the obesity epidemic, reconsidering how buildings and our urban environments are built has huge implications in our health. There are some municipalities that have embraced such action and have benefited tremendously from it.
Monday, April 5, 2010
Let's Build the Environment into It
It does not take much imagination to realize that the built environment around us, has a huge impact on our lifestyle. The built environment around us includes "urban design factors, land use, available public transportation, and the activity options for people within that space" (Booth et. al). The research backs this up, and a systematic review on "Obesity and the Built Environment" supports these relationships spot on. Some key findings of the systematic review related to the built environment include
- Overweight and obese adults were more likely to live in neighborhoods that lacked adequate sidewalks and proximal places for physical activity.
- Residents from high-walkability neighborhoods lived in neighborhoods more conducive to physical activity and had lower reported BMIs compared to low-walkability neighbourhoods.
- Residents of sprawling counties walked less, had higher BMIs, and higher obesity and hypertension prevalence than did residents of more compact counties.
- Overall, residing in a deprived area or neighborhood was associated with a higher probability of having an adverse CVD risk profile.
Sunday, April 4, 2010
Socioeconomic status and Obesity

There seems to be a lot of work done on low SES status influences obesity. There are some good systematic reviews, such as one by Dr. Lindsay McLaren from Calgary and one put out by the World Health Organization on the influence of SES indicators on obesity.
The research indicates that there is a shift from lower income countries to higher income countries as to how the different quartiles of the population which are affected by obesity. In lower to middle income countries, there is a higher association of developing obesity in the top quartiles of society. Meanwhile, in developed countries, there was a higher association of obesity with the lower SES quartiles.
Interestingly, the study found this trend more pronounced among women. According to the WHO review, "Obesity was significantly more common among women of higher SES in all low-income economies and more common among women of lower SES in all upper-middle-income economies."
The data also indicates that in the developing world, as economic growth takes place, the lower quartiles are earilest affected with increases in obesity rates. This is especially concerning as some of the economic indicators for many nations around the world rise, there is an associated rise of chronic diseases like obesity taking place with that. Dr. Mclaren partly attributes this to the barriers of healthy lifestyles in the lower income quartiles even in the face of economic prosperity coupled with sociocultural value placed on large body types in lower SES communities in low income countries.
Subscribe to:
Comments (Atom)














